paramounttpa.com Cashless & Reimbursement Claim Procedure : Paramount Health Group
Organization : Paramount Health Group
Facility : Cashless & Reimbursement Claim Procedure
Home Page :https://www.paramounttpa.com/
| Want to ask a question / comment on this post? Go to bottom of this page. |
|---|
How To Claim Paramount Cashless & Reimbursement?
Paramount Health Group Cashless & Reimbursement Claim Procedure
Obtain Cashless Facility :
Important :
We request all members who want to available cashless benefit to kindly call up our Helpline / Call Centre.
** Insured has to arrange for the Admission Request Note to be sent across from respective network hospital to Paramount.Only expenses relating to hospitalisation will be reimbursed as per the policy taken. All non-medical expenses will not be reimbursed.
** Admission request note is available on admission counter of network hospitals.
** The admission request note is to be filled in by the treating Doctor with his signature & stamped by the Hospital.
** It is mandatory for insured to mention the PHS ID on the request for proper identification / verification & further processing.
Incase Of Planned Hospitalisation (To A Network Hospital) :
Notify Paramount at least 3 days prior to the date of admission
** Kindly send the completely filled hospitalization request note either by Fax or by E-Mail.
** Claims arising from Mumbai will be handled / processed at Mumbai.
** If the ailment is covered under policy conditions, an Authority Letter would be issued to the concerned hospital
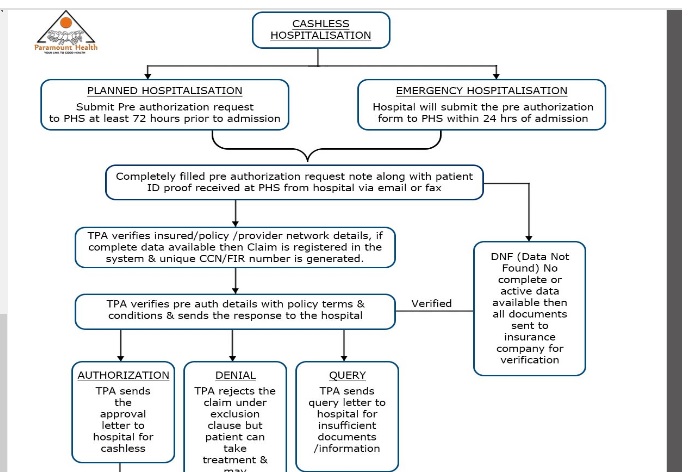
How To Obtain Cashless Facility?
The insured / patient needs to initially confirm the following details pertaining to his/her coverage with regards to :
** Policy Service Status
** Network Hospital Status
** Claim intimation
** All of the above can be confirmed with PHS Call Center or by calling the Helpline number provided on the UHID issued.
** Arrange to submit completely filled request note from respective hospital.
** Planned hospitalization should be intimated to Paramount atleast 72 hours prior to admission.
** Emergency admission to be intimated within 24 hours after hospitalization.
What To Do In An Emergency :
In an accidental case or in medical emergency you are advised to approach nearest Network / Non Network Hospital with your PHS ID Card.
Network Hospital :
If the admittance is in a network hospital, pre-intimation can be made by the claimant or relatives by calling up PHS (Helpdesk is open 24 X 7).
Non Network Hospital
If you are in non-network hospital you may pay the expenses and claim reimbursement based on policy coverage.
Paramount Reimbursement Claims
** Reimbursement claims can be submitted to Paramount Health Services & Insurance TPA Pvt. Ltd. (PHS) through courier, post or in-person at any of our branches.
** Claim Intimation needs to be given 24-48 hours prior for Planned Hospitalization & within 24 hours in case of Emergency Hospitalization.
** Claim form can be collected from the nearest Divisional / Branch Office of the Insurance Company / Paramount office. Claim forms can be downloaded here. Issuance of claim form does not amount to admission of any liability, under the policy on the part of the insurers.
** Claim Documents should be sent to Paramount Health Services & Insurance TPA Pvt. Ltd. within 7 days from the Date of Discharge.
** Documents that you need to submit for a hospitalization reimbursement claim should be as per the checklist (Checklist)
** On receipt of claim at PHS,your Claim will be scrutinized as per terms and conditions of your health insurance policy. Please note that Non-medical expenses will not be payable.(Non payable list)
** On scrutiny of your Claim if there are any further requirements for ascertaining the Admissibility, we may request for additional information. This additional information is to be submitted within the stipulated time period.
** On receipt of complete Documents, an appropriate claim decision will be recommended to your respective Insurance Company.
** On approval of admissible claim, Insurance company will directly credit your/Employer bank account with the net payable amount through NEFT.
** Upon Rejection of claim, Repudiation Letter quoting the reason for rejection will be sent to you by the Insurance Company.
Paramount Reimbursement Cases
** Reimbursement claims can be submitted to PHS through courier, post or In Person at any of our Branches
** Claim Documents should be sent to PHS within 15 days from the Date of Discharge.
** Claim form can be collected from the nearest Divisional / Branch Office of the Insurance company / PHS office. Claim forms can be downloaded from here. Issuance of claim form does not amount to admission of any liability, under the policy on the part of the insurers.
Documents that you need to submit for a hospitalization reimbursement claim are :
** Original Completely filled in Claim form
** Covering letter stating your complete address, contact numbers and email address (if available
** Copy of the PHS ID card or current policy copy and previous years’ policy copies (if any)
** Original Discharge Card/ Summary
** Original hospital final bill
About Us:
Paramount Health Services & Insurance TPA Pvt. Ltd. (PHS) began its journey in 1996. In 2002, it acquired a license from Insurance Regulatory and Development Authority (IRDA no: 006), to act as a TPA, when the concept of TPA was at a very nascent stage. Today, it is one of India’s leading Third Party Administrators (TPA).
PHS has created benchmarks in the industry with its focus on quality customer service and expertise in claims management with emphasis on checking fraud and abuse. It operates in 155+ locations in India touching many lives each day with its bouquet of services.
Some Important Information From Comments
Comments:
1. I have enrolled my name for the health insurance scheme being implemented for SBI Retirees and expecting card shortly. While, I stay at Pune I draw my pension at Mumbai. I request to guide me if the card issued at Mumbai is valid any where in India?
2. Our health insurance claim process is simple and easy. In case of hospitalization, you can avail cashless facility at our 4300+ network hospitals. Our proficient and skilled staff will do all it needs to make sure that you get your compensation as quickly as possible. To serve you better, we have tied up with the two main Health claims handlers, Paramount and Emeditek.
FAQ On Paramount Reimbursement
Sure, here are some FAQ on Paramount Reimbursement:
What are the documents required to submit a reimbursement claim?
The documents required to submit a reimbursement claim are:
** Original completely filled & signed IRDA Claim form.
** Covering letter stating Schedule of Expenses.
** Copy of the PHS ID card or current policy copy and previous years’ policy copies (if any).
** Original bills and receipts from the hospital or doctor.
** Any other documents that may be required to support your claim, such as a doctor’s report or a letter from your employer.
How long does it take to process a reimbursement claim?
The processing time for a reimbursement claim varies depending on the complexity of the claim and the number of claims that Paramount is currently processing. However, most claims are processed within 4-6 weeks.
What happens if my claim is denied?
If your claim is denied, you will receive a letter from Paramount explaining why your claim was denied. You may appeal the denial by submitting a written appeal to Paramount.
I have Submitted My Reimbursement Claim File on 23 July 2022.
Today 22 August 2 022. Approximate 1 month Completed. Butt Still amount not settled.
Payment Settled time need to be improve.
I furnished below the claim details & even after 1year 2months this is not settled. Name of Insurance Company:National Insurance Company
PHS ID : 21614909
Office Name : Delhi do
Name of Beneficiary : MARY THOMAS
Policy Number : 354800/46/15/8500000041
Name of Employee : SHEEBA VALLOOR BABY
Group Name : FORTIS HEALTHCARE LTD
Policy Period : 01/05/2015 to 31/05/2016
Employee Number : 110251
Gender : Female
FIR DATE :05/10/2015
FIR NO :2924655
What is the format for intimation in case of non network hospitalization?
I need guidance for hospital admissions.
My wife is suffering from kidney failure and she is undergoing continuous ambulary peritoneal dialysis. Can I get reimbursement?
I am Santosh Kumar Singh. I admitted in Irone Hospital Kalkajee on 25th July 2016 and discharged on27th July but paramount regional office okhlla phase 1 send all reimbursement paper by India post spreed post. My policy no. is23825097. Please show the status.
23693366 is my I’d no. I want to know why prostate treatment is not Included in policy, while maximum numbers of pensioners are sufferered in the old age.
My son Srinivas id no is 871411. Can you send the claim details/ intimation since hospital insurance cell works only to 9am -6pm. Now he was admitted in Chennai base hospital. Tell current details please.
I furnish below the claim details & even after one month this was not settled:-
Claim Details :
Name of Insurance Co : United India Insurance
Company PHS ID : 23586737
U/W Office Name : CORPORATE CELL MUMBAI
Name of Beneficiary : S RAMAMURTHI
Policy Number : 500100/48/15/41/00000522
Name of Proposer/Employee : R MANGALAM
Group Name : UNION BANK OF INDIA (RETIRED)
Policy Period : 06/11/2015 to 31/10/2016
Employee Number : 37923
Gender : MALE
Address : No 5/2 Third Main Road, Pukhraj Nagar Madhavaram, Chennai 600060 Chennai Tamil Nadu 600060
Relation : Husband.
Claim Registration
Name of Provider :THE MADRAS MEDICAL MISSION.Processing Branch :044
Insurer CCN : 0 Date of Admission : 17/02/2016
FIR Date : 10/03/2016.Date of Discharge :19/02/2016
FIR Number : 3074645 Al/Denial Date : –
FIR Extention : Al Amount: 0
Partial Payment Seq: 0 Additional Al Amount: 0
Deficiencies : 1.Require attested final bill of first insurance company/TPA,where part payment was made 2.Require detailed working of claim amount settled by first insurance company/TPA with Break-up & cost of each 3.Require attested copies of all claim papers submitted to first insurance company/TPA.
4.Require ID proof and Address proof for the patient and employee.
Date of File Received : 10/03/2016
Claim Processing :
Bill Received Date :Amount Cleared :0
Provider Bill Amount : Amount Cleared Beneficiary :0
Pre/Post Provider Bill Amount : Amount Cleared Provider :0
Total Amount Claimed : Discharge Voucher Sent Date : –
Processing Status :Deficient ClaimClaim Processed Date : –
Discharge Voucher received Date.Not Payable Expenses : 0
I have enrolled my name for the health insurance scheme being implemented for SBI Retirees and expecting card shortly. While I stay at Pune I draw my pension at Mumbai. I request to guide me if the card issued at Mumbai is valid any where in India?
Regards
From the Website :
My claim number is 3050157. Which documents need to be submitted?
Our health insurance claim process is simple and easy. In case of hospitalization, you can avail cashless facility at our 4300+ network hospitals. Our proficient and skilled staff will do all it needs to make sure that you get your compensation as quickly as possible. To serve you better we have tied up with the two main Health claims handlers, Paramount and Emeditek.
My claim no is 3004882 under policy No.NA CHE40008611 I H O P. How do I find the present status of my claim? When it will be settled?
Already 15 days passed.
I am State bank of Hyderabad retired pensioner insured amount debited on 07/11/2015
When i will get ID card?
Please tell how much amount claim approved before and after hospitalization
I want to know regarding cashless eye hospital in mumbai.
My PHS ID NO:NA
MUM 22854291 JIO.
Let me know the name of the enlisted hospitals or nursing home at salt lake, kolkata to get cashless benefit from the policy already made with you.
Policy no.104200/48/15/8500001554
I want to know the list of hospital for cashless under government employees
I need the name of Cashless Hospitals within Hooghly District (West BengaL) and Kolkata (WB).
My PHA ID No. 01 KOL 20367287 CTDC W
Please send me the same..Regds
Vivekananda